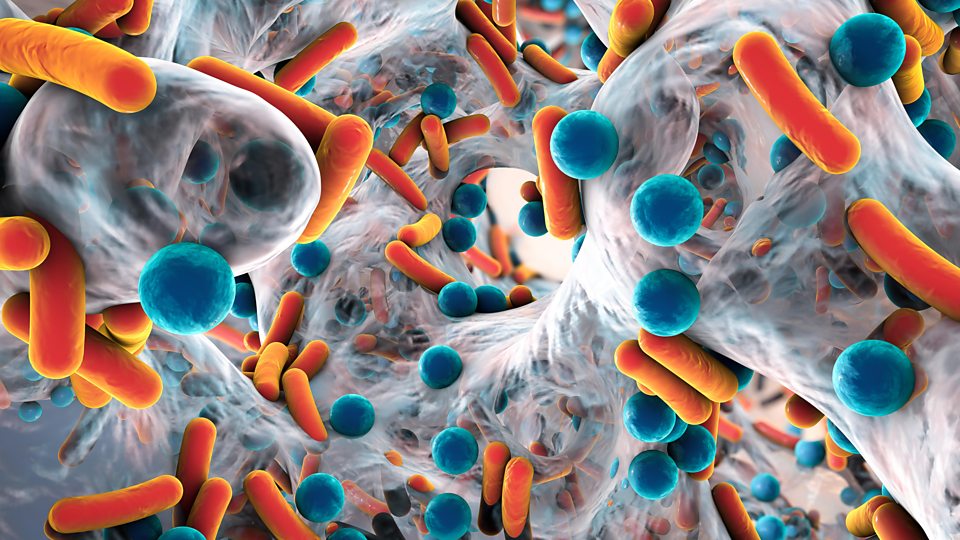
The end of modern medicine?
A glimpse of the future
Humans are at risk for exposure to new resistant pathogens or resistance determinants from animals through direct contact, ingestion of contaminated food or water, and contact with infected humans.
Humans and other animals can acquire resistant pathogens and commensal organisms simply by ingesting them. Contaminated meat and other cross-contaminated foods cause millions of cases of gastrointestinal illnesses such as salmonellosis and campylobacteriosis each year in the USA alone (Scallan et al.2011).
Following exposure of humans-to-resistant organisms from agriculture, there may be further spread within the human population. Varying degrees of onward transmission within humans have been documented for different clonal types of methicillin-resistantStaphylococcus, originally acquired from livestock. This possibility for animal-to-human transmission, in the case of MRSA ST398, brings heightened concerns about livestock as potential reservoirs of zoonotic infections that may with further evolution become adapted to circulation within the human population”
🔗 Source: Antibiotics in agriculture and the risk to human health: how worried should we be?
Resistant Staphylococcus aureus strains are spreading between pigs, farmworkers, their families and community residents, and represents an emerging
Antibiotic resistant strains of staph bacteria may be spreading between pigs raised in factory farms. DNA sequencing of bacteria found in pigs and humans in rural eastern North Carolina, an area with concentrated industrial scale pig farming, suggests that multidrug resistant Staphylococcus aureus strains are spreading between pigs, farmworkers, their families and community residents, and represents an emerging public health threat, according to a study led by researchers at the Johns Hopkins Bloomberg School of Public Health.

🔗 Source: Antibiotic-resistant strains of staph bacteria may be spreading between pigs raised in factory farms - Findings from DNA-sequencing study raise public health concerns
And the current practice of modifying current antibiotics - won’t be enough
The pharmaceutical industry is mostly limited to modifying current antibiotics to combat growing resistance.
Soon this method won’t be enough to keep the resistant bacteria at bay…..
A world without antibiotics could see the resurgence of old illnesses such as tuberculosis (TB), typhoid fever, pneumococcal disease and diphtheria which claimed millions of lives before penicillin was invented. In fact, a drug-resistant TB strain known as XDR-TB is currently on the rise in Europe and is extremely difficult to treat, with only one third of cases successfully cured. Also, sexually-transmitted bacterial infections such as syphilis and gonorrhoea, which are currently treated with a simple course of antibiotics, could turn into serious health threats. There has been a recent global outbreak of super- gonorrhoea that is resistant to both antibiotics used to treat the infection.
Treatments for diseases that the pharmaceutical industry has spent decades trying to develop, such as cancer, may become much less effective. Before the age of antibiotics, the simplest of cuts could be fatal if infected with bacteria, meaning that surgery was very risky. Without effective antibiotics, the principal ways to treat cancer - surgery - may not be as possible anymore. Other important medical procedures such as organ transplantation, chemotherapy, radiotherapy, hip replacements, cosmetic surgery and caesarean sections will become more dangerous.
Lack of antibiotics may also make natural childbirth a real risk for woman and new-born babies again. Until the 1930s, the risk of mothers and children dying during childbirth was high until antibiotics caused mortality rates to plummet. Today, over 30,000 women and 400,000 new-borns in developing countries die every year due to infections relating to birth, of which 200,000 infants die from multi-drug resistant infections. Although birth mortality rates are low in high-income countries today, continued overuse of antibiotics will lead to antibiotic resistance, making childbirth complications harder to treat with available drugs.”